LDL used to be the “bad cholesterol” and HDL the “good cholesterol.” That’s the tidy story I learned in my grad school lipids class 13 years ago, but the science has evolved since then. High HDL is no longer automatically good, for example. Let’s take a look at what your cholesterol numbers really mean.
The most common way you’ll get these numbers, called a lipid panel, gives you a report of your total cholesterol, LDL, HDL, and triglycerides. The results might lead to a high five from your doctor or a serious sit-down to talk about “lifestyle changes” and even cholesterol-lowering medications. It is recommended that you get your lipids checked at least every five years and more frequently if your numbers indicate any concern.
The lipid panel is one of the primary ways that doctors keep tabs on your risk of developing atherosclerosis, the formation of fatty plaques in the walls of arteries, which narrow and harden these blood vessels and increase the chance of a piece of plaque or a blood clot blocking blood flow. This can cause damage anywhere in the body, but if it happens in a coronary artery of the heart, you can end up with a heart attack. If it happens in the brain, you can end up with a stroke.
Atherosclerosis is partly caused by the cholesterol and triglycerides (fat) circulating in your blood, and the lipid panel is like a window into how much cholesterol is circulating and what it’s up to.
Total Cholesterol Isn’t the Important Part
It’s not fair that cholesterol has become sort of a dirty word, because it’s a vital molecule in the human body. It’s an important component of cell membranes, part of bile (needed for fat digestion), and a precursor to vitamin D and some hormones, including cortisol, estrogen, and testosterone.
Just because cholesterol is important doesn’t mean we need to eat a ton of it. In fact, we don’t need to eat it at all, because our bodies can make all the cholesterol that we need. But unless you’re vegan, cholesterol is also part of your diet, being present in foods with animal fats, like meat, fish, eggs, milk, and butter. For decades, dietary guidelines recommended that we limit how much cholesterol we consume, but we now know that the amount of cholesterol we eat has little impact on the amount in our blood, because the body’s cholesterol synthesis decreases if we eat a lot of cholesterol. With that said, you should still limit saturated fats in your diet. Most animal fats are also high in saturated fats – eggs and fish being notable exceptions.
Your blood lipid results will give you a value for total cholesterol, but this number doesn’t mean much on its own. On its website, the American Heart Association (AHA) doesn’t even give a range for normal total cholesterol, saying, “Nowadays, these ranges aren’t used. Instead, total cholesterol levels are considered in context with other risk factors, and treatment is recommended accordingly.”
Traditionally, total cholesterol under 200 mg/dL has been considered healthy, and Dr. Ali Rahimi, a cardiologist with Kaiser, says he still likes to see total cholesterol under that mark.
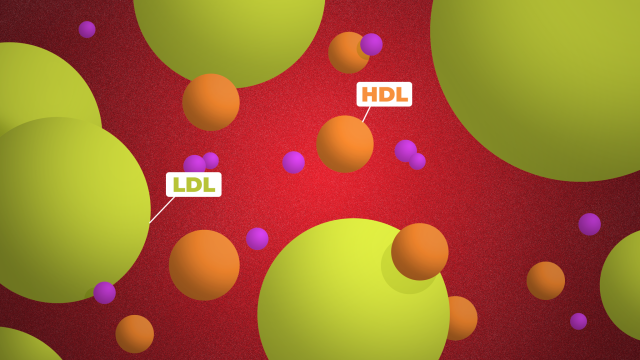
But more important than total cholesterol is how it is packaged and where it’s headed in the body. That brings us to LDL and HDL. They’re both types of lipoproteins, the transport vehicles that shuttle cholesterol and other lipids through the blood, but they each have different jobs and thus different effects on our health.
The bottom line: Ideally this number will be below 200 mg/dL, but total cholesterol doesn’t really mean much; the other numbers in your report are the ones that matter for your health.
LDL Is Lousy
LDLs are loaded up with cholesterol, because their job is to deliver cholesterol from the liver to all the other cells that need it. It’s an important job, but LDL can also initiate atherosclerosis, so too much circulating in blood isn’t a good thing. That’s where LDL’s “bad cholesterol” reputation comes from, and it’s probably warranted. People with high LDL are more likely to develop atherosclerosis and heart disease, and lowering LDL with medication (usually statins) or lifestyle changes reduces that risk.
Your doctor or lab results will probably say that LDL should be below 130 mg/dL. However, cardiologists are using this value in a more nuanced way than they did five years ago. “Before, we were very, very focused on looking at the exact number and thinking that lower is better, and then we would initiate pharmacotherapy at certain [higher] levels,” said Rahimi.
If your LDL is above 190 mg/dL, that’s considered very high, and the AHA recommends treatment with a statin regardless of other factors. But below that number, the AHA considers LDL as one risk factor among many, including things like smoking, diabetes, high blood pressure, and a family history of premature coronary heart disease, all of which raise your risk of heart disease and might increase the urgency of taking medication to bring cholesterol down. These are things to discuss with your doctor, but you can also use this online calculator to tally up your risk.
Rahimi says an LDL of less than 130 is the goal, and if you fall somewhere between 130 and 190, whether or not he recommends medications depends on all of those other risk factors. But regardless, people in this range can benefit from stopping smoking, getting more exercise, and improving their diet, and Rahimi prefers to start with this approach if possible. These changes can decrease your LDL by as much as 30 mg/dL, he says, and that’s an incredibly helpful jump whether you end up needing a cholesterol-lowering medication or not.
The bottom line: LDL is still the “bad” cholesterol, and a good result is under 130 mg/dL. Lifestyle changes and medication can both help, and you’re very likely to be prescribed medication if your LDL is above 190 mg/dL.
HDL Isn’t as Helpful As Hoped
HDL has long enjoyed a charmed reputation. It cleans up old and excess cholesterol around the body – including from fatty plaques in arteries – and returns it to the liver for recycling and disposal. People with lower HDL tend to have a higher risk of cardiovascular disease, so the obvious conclusion was that more HDL must be better. (Traditionally, a healthy HDL level has been 40 mg/dL or higher for men and 50 mg/dL or higher for women.)
But this is where the science has been surprising over the last few years. There was hope that several drugs that raise HDL would help prevent heart disease, but they failed in clinical trials. (In fact, some turned out to cause more harm than good.) Genetic studies have also found that having genes that raise HDL doesn’t necessarily protect us from heart disease.
“That’s been a big “Aha!” moment in cardiology,” said Rahimi. “We’ve kind of had to rethink [HDL], and as opposed to it being causal, it may be more of an associated factor.”
In other words, if you have high HDL, it may or may not indicate that you have a lower risk of heart disease, because there are some genetic causes of high HDL that actually increase heart disease risk.
Likewise, if you have low HDL, it may indeed mean that you have an increased risk of heart disease, but probably not because of your lack of HDL. “It’s kind of like a marker,” said Rahimi. “People who have low HDL are more likely to be sedentary, may be smokers, may have more insulin resistance,” so your doctor may talk about addressing those issues rather than trying to raise HDL as an end goal.
“The classic ‘good cholesterol, bad cholesterol,’ is really out,” said Rahimi.
HDL is still an active area of research, though. Scientists are working on measuring different types of HDL to see if some are more helpful than others, and genetic tests might someday be able to help us better interpret our lipid panel numbers.
The bottom line: For now, HDL is probably not a very useful number.
Triglycerides Tell a Story, Too
The last value you’ll see on your lipid panel is for your triglycerides. Normal triglyceride levels are less than 150 mg/dL, and higher values are associated with increased risk of heart disease. (Unlike HDL, this association has held up in genetic studies, but there’s less research on triglycerides overall.) However, Rahimi says that it isn’t until triglyceride levels are above 500 mg/dL that he starts to consider medications. (Drugs used include statins, fibrates, niacin, and high-dose fish oil.) Between 150 and 500, he talks about lifestyle changes to lower triglycerides.
“When we see higher triglyceride levels, we get concerned about the person’s diet,” Rahimi said. One of the major drivers of high triglycerides is carbohydrate intake, especially sugar. Obesity and insulin resistance, which can lead to diabetes, also causes increased triglyceride levels, as does excess alcohol intake.
The bottom line: Triglycerides should ideally be below 150 mg/dL, and you can lower that level through diet. Above 500 mg/dL you’ll likely be prescribed medication.
Little Numbers, Big Picture
The blood lipid panel remains a primary method of assessing risk of heart disease. What’s nice about these values is that they’re quantitative and trackable over time. However, they also have limitations. Some lipid values are more useful than the others, and none exist in a vacuum. They’re affected by many factors, some that you can change, and some that you can’t, including genetics. We’re still trying to understand them, and we probably should have known better than to think biology could be as black and white as good cholesterol and bad cholesterol.
Comments
4 responses to “What Your Cholesterol Numbers Really Mean”
This gets a “thumbs up” as well as a “thumbs down”.
Thumbs up first:
For years, I’ve seen American TV shows with characters saying they had a cholesterol reading of 200. And I’d always wonder: 200 what exactly? Now I know: mg/dL.
Thumbs down:
Last time I had an Australian cholesterol test, my GP had a talk because I had a “high” reading of 6. 6 mg/mol, from memory (what’s a mol? No clue)
The point being – it’s great to have health articles, it’s extra great when you include the unit of measurement. But when the measurements in Australia use a different unit, you really should throw in a conversion factor.
mol (Mole) is a specific number of molecules/particles used in chemistry.
https://en.wikipedia.org/wiki/Mole_(unit)
As jaysevento noted, the correct Aussie unit is mmol/L . A mol is a count of molecules (1 mol = 12g of carbon-12 = 6.023 x10^23 atoms).
I guess different types of cholesterol have unique weights, so our unit is a variation of “parts per million”. A particle count does make more sense than a weight measure.
This is obviously taken from a US article, as we use mmol/L in Australia/NZ.
There’s also more than one type of LDL – you only need to be concerned with the small dense particles.
Lastly, the only thing you need to be concerned with is having your Triglycerides 1 or under, and a good HDL/TR ratio.
Google “The Great Cholesterol Myth” by Jonny Bowden – an interesting read if you think you have high cholesterol.